

The Facility Assessment Study conducted by India Health Action Trust (IHAT) in 25 High Priority Districts (HPDs) of Uttar Pradesh (2013), showed that there were significant gaps in facility preparedness for providing Reproductive, Maternal, Newborn and Child Health (RMNCH) Services. The primary care level facilities – Primary Health Centers (PHCs) and Community Health Centers (CHCs), which accounted for nearly 70% of all public health deliveries, were not adequately prepared for providing basic emergency obstetric and newborn care. Less than 20% of the clinical providers – Auxiliary Nurse Midwives (ANMs) and Staff Nurses (SNs) had been trained as Skilled Birth Attendants (SBAs). The availability of essential newborn services such as newborn resuscitation, phototherapy for newborn and Vitamin K for newborns, was low. There was also a shortage of essential medical supplies such as uterotonics, anti-hypertensive, injectable ampicillin and injectable gentamicin1.
These findings pointed to the need to strengthen various aspects of facility preparedness for the provision of RMNCH services, including the need to strengthen the referral system for pregnant women and newborns with complications. Acknowledging this urgent need, Uttar Pradesh Technical Support Unit (UP TSU), a Unit implemented by IHAT, in partnership with University of Manitoba (UoM and launched the Nurse Mentoring Program in 2014, beginning with 150 blocks of 25 HPDs in Uttar Pradesh.
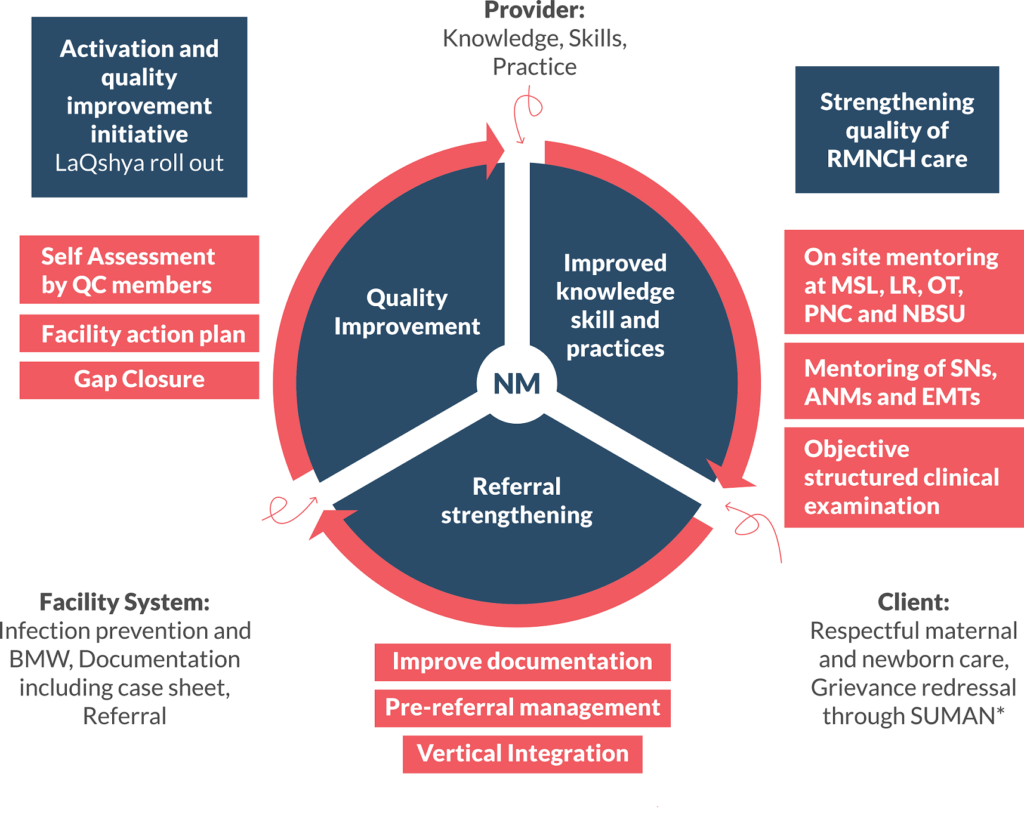
The Nurse Mentoring program aimed to improve knowledge, skills and practices of the staff nurses around mother and newborn care, intra partum and post-partum care and management of maternal and new born complications, through its dedicated workforce/change agents called Nurse Mentors (NMs). The strategy involved creating a cadre of nursing professionals (Nurse Mentors) to improve the quality of care around birth in the facilities. This cadre was supported by a group of qualified public health professionals at district and zonal level, who provided mentoring and managerial support to the NMs and played a key role in supporting the health administration in systems strengthening at facility level. At the state level, program policy design, monitoring and clinical specialists were actively engaged in the program development.
Nurse Mentors are a new cadre of nurses trained in clinical skills and quality improvement processes in a labor room setup. They strengthen the clinical competencies of the staff nurses and ANMs and also facilitate improvement in system level components. The NMs are posted at sub- district block facilities and District Women’s Hospitals, where they work with health facility administration, staff nurses/labor room service providers and outreach ANMs to enhance the quality of care across the continuum of care for mother and newborn.

The NMs anchor the Nurse Mentoring Program and work towards improving upon five key clinical competencies of staff nurses and five critical facility systems as below:
Clinical competencies of staff nurses
Systems Strengthening at the facility level
The major components of the Nurse Mentoring Program include (Figure 1):
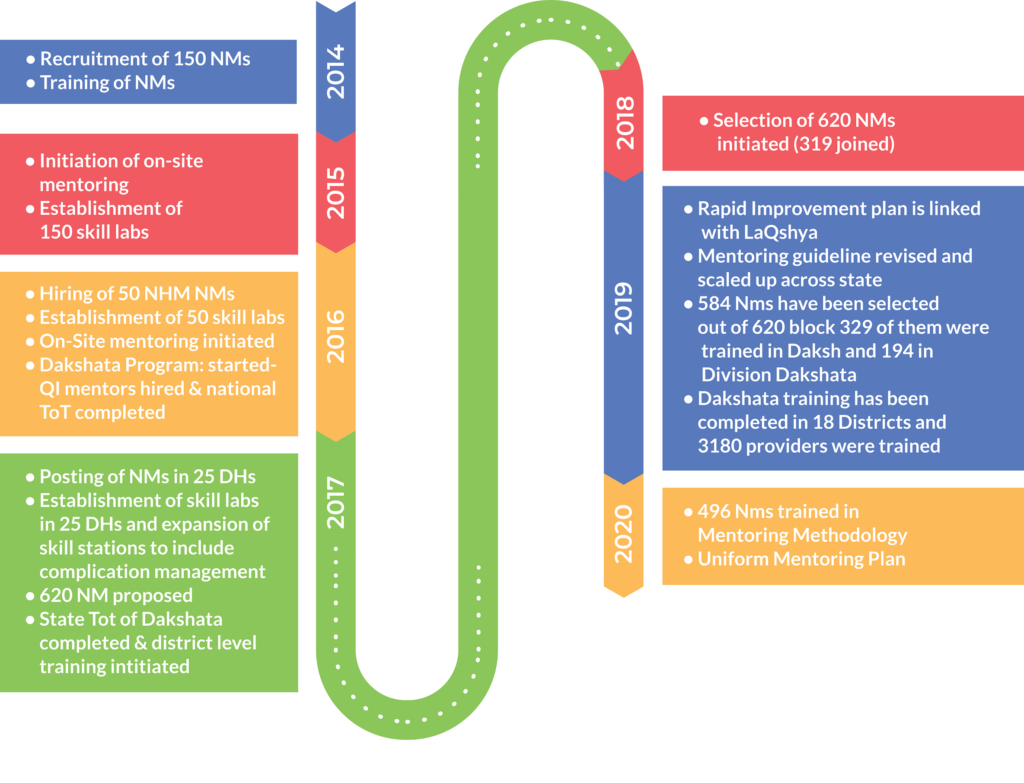
Coverage and Chronology
The NM program initially started in 2014 -15 placing one NM in each of the 150 blocks of 25 HPDs. In 2016, the program expanded to cover 50 more blocks within the HPDs. In 2017, through advocacy meetings with the government, the program again expanded its coverage to cover the 26 district women hospitals and centers/tertiary level facilities in 25 HPDs of UP. This intervention catered to around 61% of delivery load in the public sector. Outside the HPDs, the Dakshata program of Government of India (GoI) has been operational in 31 districts of UP since 2016, where 124 facilities with 40% of the public sector delivery load are being covered through district level Quality Improvement mentors. Seeing the positive results of the program in 2018, GoUP, scaled the program to remaining 620 blocks in 75 districts through nominated nurse mentors selected from amongst existing staff nurses (Figure 3). Over a period of 5 years, the NMs have mentored over 2400+ staff nurses and 800+ ANMs in 25 HPDs, covering 240 facilities including 26 District Women Hospitals. In 2019, the program is being scaled up in all 820 blocks of 75 districts of Uttar Pradesh with nominated nurse mentoring model.
Rolling Facility Surveys were conducted to assess the output of the program; whereas, external monitoring and evaluation agency was engaged to assess the outcomes of the program.
Key Achievements
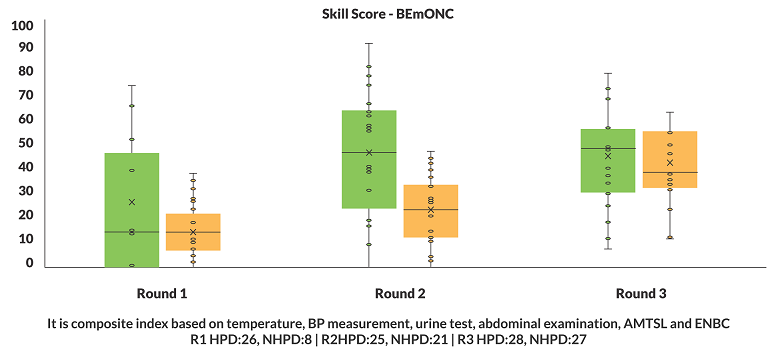
(a) Improved clinical competency of SNs and ANMs: There is significant improvement in the composite index based on the indicators – temperature, blood pressure, urine, abdominal examination, AMTSL and ENBC, over a period of time from round 1 and round 3. Median score has reached above 50 percent in HPDs as compared to less than 40 in Non HPDs (Figure 3).
(b) Improvement in knowledge/skill and clinical practices of intrapartum care: Composite index was calculated based on 8 knowledge/skill and 9 clinical practice indicators. There is a significant improvement of skills, knowledge and practice in last 2 Rolling Facility Survey (RFS) round conducted between 2017 and 2019 (Figure 4).
(Each bubble represents the delivery points and size is an indicator of delivery load. Dark blue bubbles represent optimization blocks whereas light blue, pink and orange represent NHM NMs facility where implementation started later).
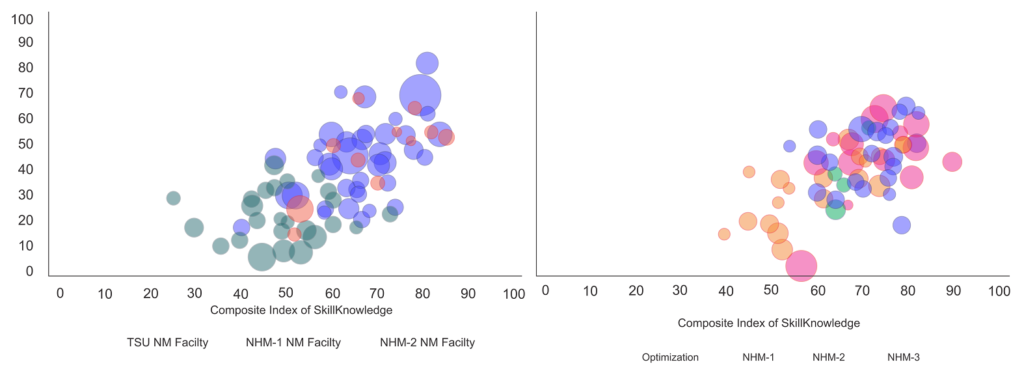
In RFS 4, it was observed that National Health Mission (NHM) NM facilities are catching up the blocks, where UP TSU had deployed the NMs and there is a clustering of facilities in right upper quadrant showing improvement in skill, knowledge and practice with few outliers with facility having poor practices although skills are on higher side.
(d) Changes in labour room practices: The Nurse Mentoring Program resulted significantly in improved routine labour room practices that have a high potential of reduction in maternal and newborn deaths including AMTSL (which prevents postpartum hemorrhage (PPH) and its consequent case fatalities) and routine newborn care (which can significantly reduce the number of newborn deaths).
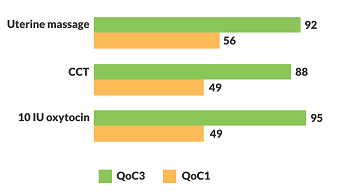
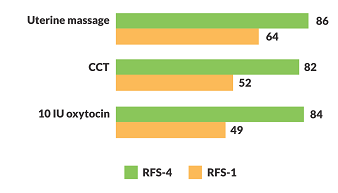
The RFS and external MLE data shows that, there was considerable improvement in different steps in active management of third stage of labour (AMTSL which by itself can prevent 70% of maternal deaths due to PPH2). The most important step of AMTSL (administration of 10 IU oxytocin) improved from 49% in 2015 to 95% (94%) in 2019 as per External MLE data and from 49% in 2014 to 84% (71%) in 2019 as per RFS data (Figure 5 and 6).
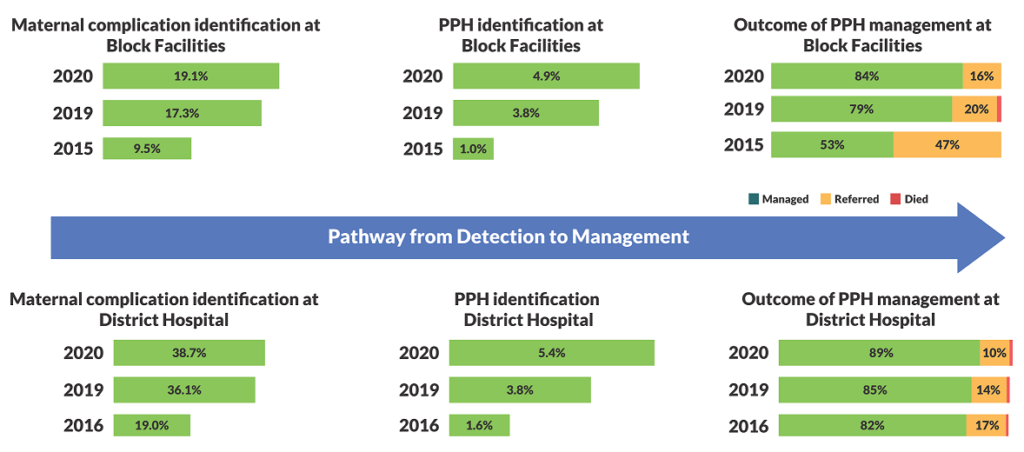
(e) Improvement in detection and management of maternal and newborn complications: Figure 8 shows that the rate of identification of maternal complication increased from 19.0% in 2016 to 34.0% in 2020, the detection of PPH increased from 1.6% to 5.4% with 70% reduction in referral out at district hospital level. The changes at block level facilities for detection of maternal complication, PPH detection and referral out of PPH cases changed from 9.5% to 19.1%, 1.0% to 4.9% with 66% reduction in referral out of PPH cases between 2015 and 2020.
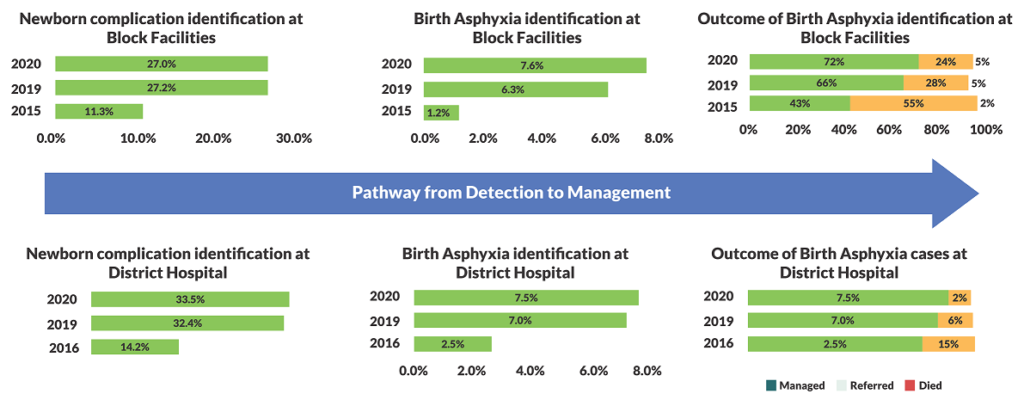
Similarly, Figure 9 shows that the rate of identification of newborn complication jumped from 14.2% in 2016 to 33.5% in 2019, the detection of birth asphyxia increased from 2.5% to 7.5% with 87% reduction in referral out of birth asphyxia cases at district hospital level. The changes at block level facilities for detection of newborn complication, birth asphyxia detection and referral out of birth asphyxia cases changed from 11.3% to 27.0%, 1.2% to 7.6% with 56% reduction in referral out of birth asphyxia cases between 2015 and 2020.
(f) Referral strengthening: Vertical Integration meetings and leveraging technology platforms have enhanced referral strengthening process. The VI meetings have resulted into the following outcomes:
Thus, as a result of the Nurse Mentoring Program a substantial shift in detection and management of maternal and newborn complications can be clearly observed at district hospitals and block level facilities, thus, equipping facilities to manage such complications and facilitate the reduction in maternal and neonatal mortality across the state.
Based on the learnings from the Nurse Mentoring Program in 200 Blocks of 25 HPDs, Government of India approved the scale up of the program in all the 820 blocks of all 75 districts of Uttar Pradesh. The program has already initiated this transition. The dedicated NMs at the District Hospitals will be replaced by QC mentors/ NHM NMs in 2 years’ time. Mini skill labs will be established in remaining 620 block facilities and all DWHs across state. Uniform mentoring plan across the state will be developed/operationalized.

“The Nurse Mentoring Program has helped the
staff nurses immensely, in managing maternal
and neonatal complications at the facility. The
Nurse Mentor posted here, at DCH Manjhanpur,
Ms Sharda (name changed), not only provided me with a mentoring drill and demonstration at the Mini Skill Lab, but also gave me hands-on training during actual delivery cases. This increased my c o n fi d e n c e o n m a n a g i n g m a t e r n i t y complications by my own self. Day-to-day capacity building process and mentoring by Ms Sharda during monthly Quality Circle Team meetings ensured timely decisions to address the persisting gaps at the facility. Ms Sharda also supported in the LaQshya and National Quality Assurance Standards initiatives.
“I have been posted as the Chief Medical
Superintendent at the District Women’s Hospital at Hardoi since 2018 and have witnessed the transformation in the hospital since the implementation of the Nurse Mentoring Program. This program is highly comprehensive and tackles all the critical aspects like Maternal Death Surveillance and Response, OSCE, Post Natal Care, UPHMIS, and referral follow up, among others. The competency development of the staff nurse and improvement in facility system under the program has led to optimum functioning of the facility, thus serving the community with the right kind of services at the right time, resulting into a positive and safe birthing experience.”

1The 2013 facility assessment study, IHAT
2Prata N, Bell S, Weidert K, Prevention of postpartum hemorrhage in low-resource settings: current perspectives, International Journal of Women’s Health, 2013, Doi: 10.2147/IJWH.S51661