

Maternal, newborn and child health care is a top priority and is critical for the development of a country. Services to pregnant women are a vital component of reproductive health care1. In 2017, India contributed 15% of global maternal deaths2. The Empowered Action Group (EAG) states have the highest Maternal Mortality Ratio (MMR) and contribute to 71% of infant mortality in India.
Madhya Pradesh (MP) has made significant progress with maternal and child health interventions. However, as one of the EAG states, maternal, neonatal and under-5 mortality remains sub-optimal. MP has the highest neonatal (35/1000 live births), infant (48/1000 live births) and under-5-mortality (56/1000 live births) and the third highest maternal mortality ratio (173/100000 live births) among the larger states in India.
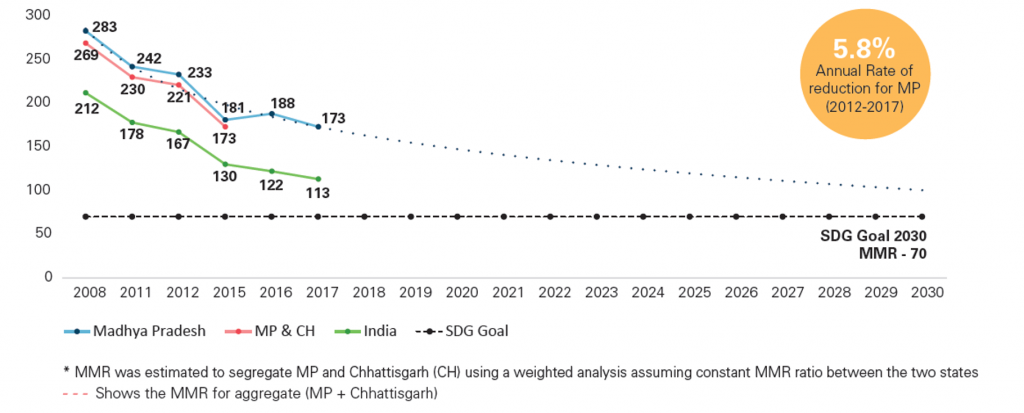
The MMR in MP and India has declined in the last decade (Figure 1). However, the Annual Rate of Reduction (between 2012 and 2017) in Madhya Pradesh (5.8%) was lower than that of India (7.5%). While India may achieve the Sustainable Development Goal of < 70 per 100000 live births by 2030, MP may require a longer period of time.
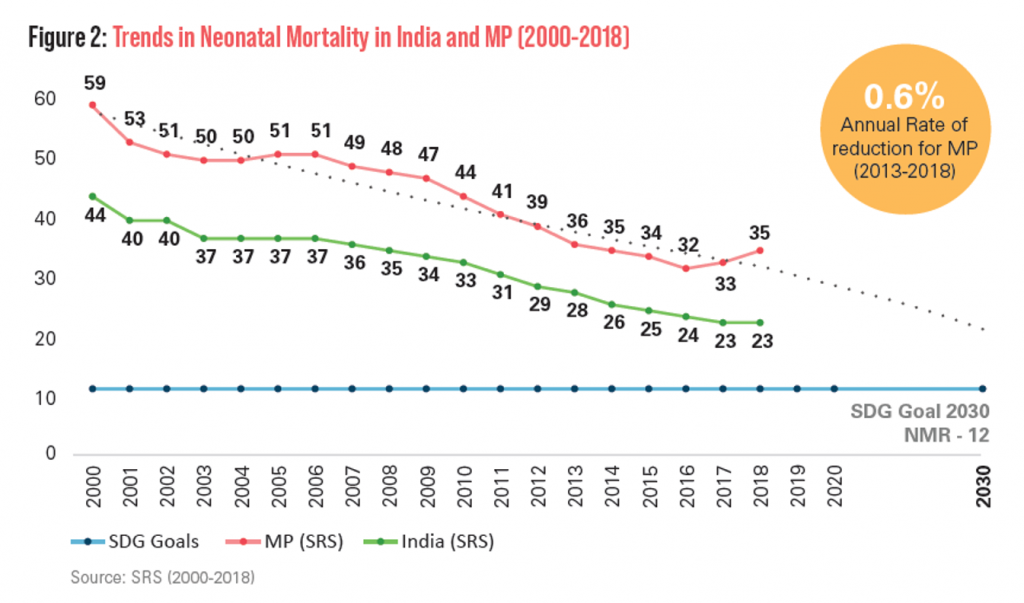
Similarly, the Neonatal Mortality Rate (NMR) has been declining in MP and India in the last decade (Figure 2). The Annual Rate of Reduction (between 2013 and 2018) in MP (0.6%) was lower than that of India (3.8%).
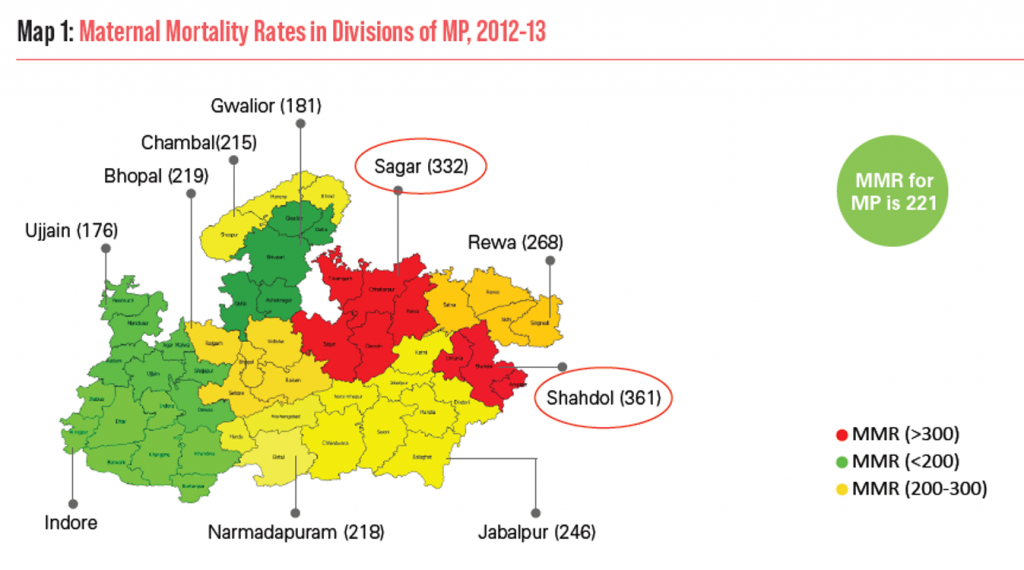
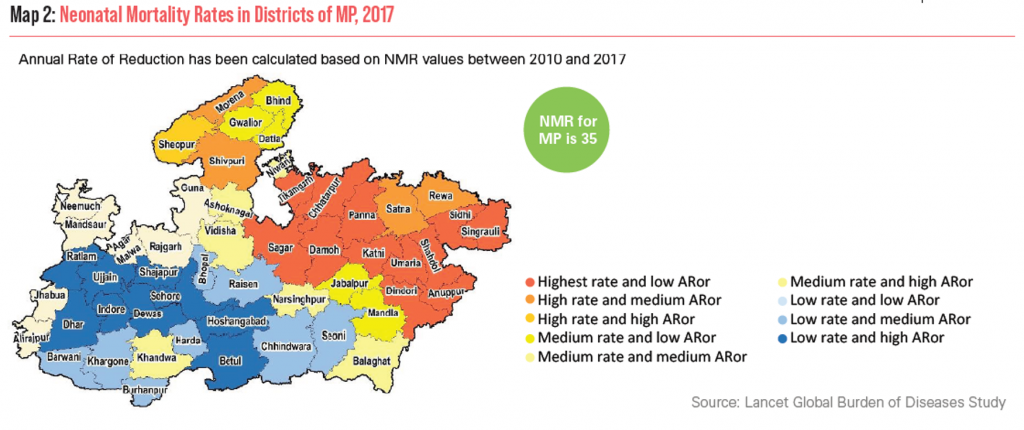
The distribution of maternal mortality in divisions within MP is uneven (Map 1). The north eastern region of MP has higher MMR; with Shahdol3 and Sagar divisions4 having highest Maternal Mortality Rates. Similarly, the district-wise distribution of neonatal mortality, using a composite indicator categorizing NMR as high, medium and low and the AARC also depicts the heterogeneity of neonatal mortality within MP (Map 2). Again, it is observed that the north-eastern part of MP (NE MP) has high NMR and a low Annual Rate of Reduction.
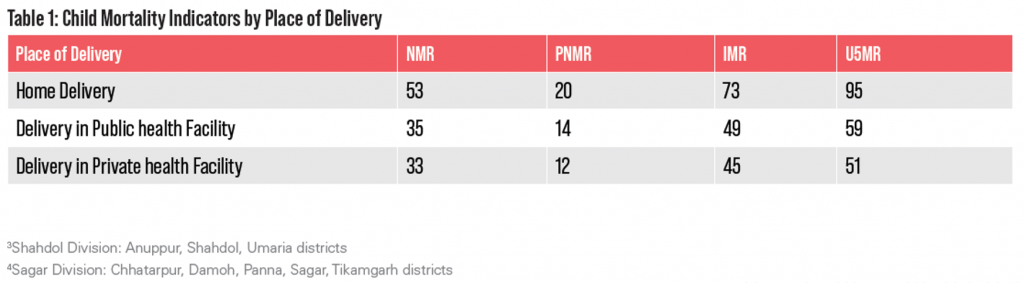
To reduce maternal and newborn mortality, high coverage and quality of services for institutional delivery is critical. However, almost one in five pregnant women in MP deliver at home. NMR, IMR, and U5MR are highest among women who delivered at home (Table 1).
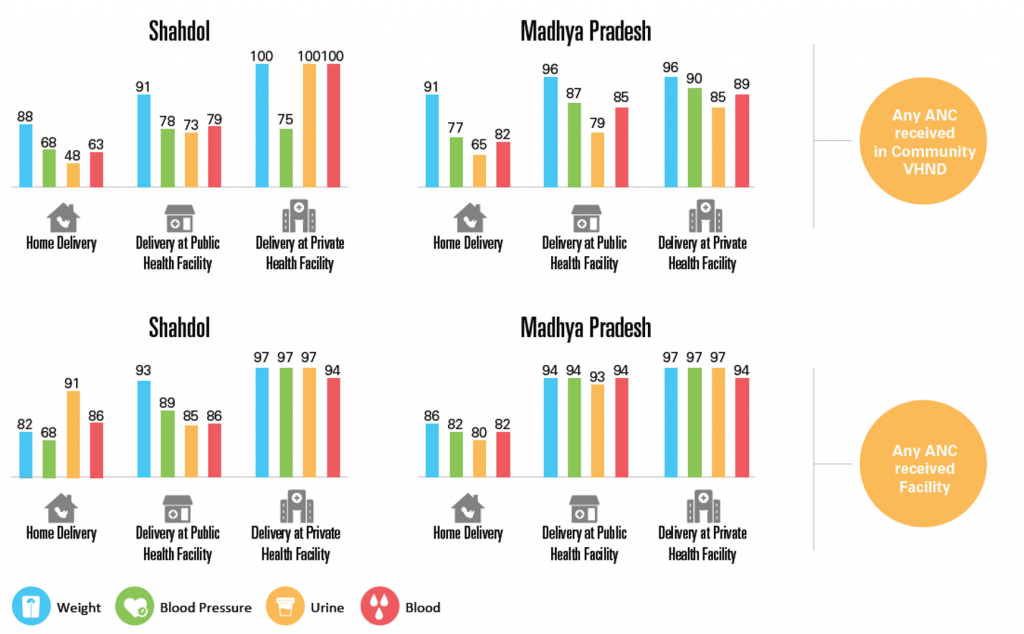
Coverage of antenatal care (ANC) services among pregnant women who deliver at home in Shahdol is much lower than among women who deliver in a health facility (public or private), across the state of MP. This is irrespective of whether the ANC services were received within a facility or in a Village Health and Nutrition Day (VHND)/community setting (Figure 3).
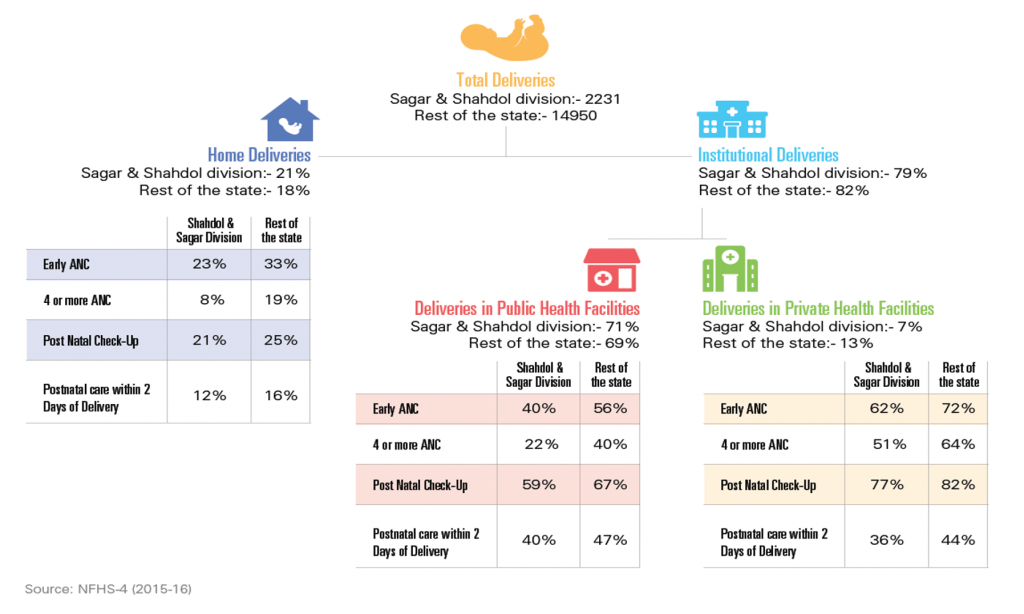
NFHS-4 data cascade analysis shows that the coverage of quality ANC and post-natal care (PNC) services such as early ANC (ANC in the first trimester), four or more ANC, post-natal check-up and early PNC are all lower in Shahdol and Sagar division and are lowest for those who deliver at home (Figure 4).
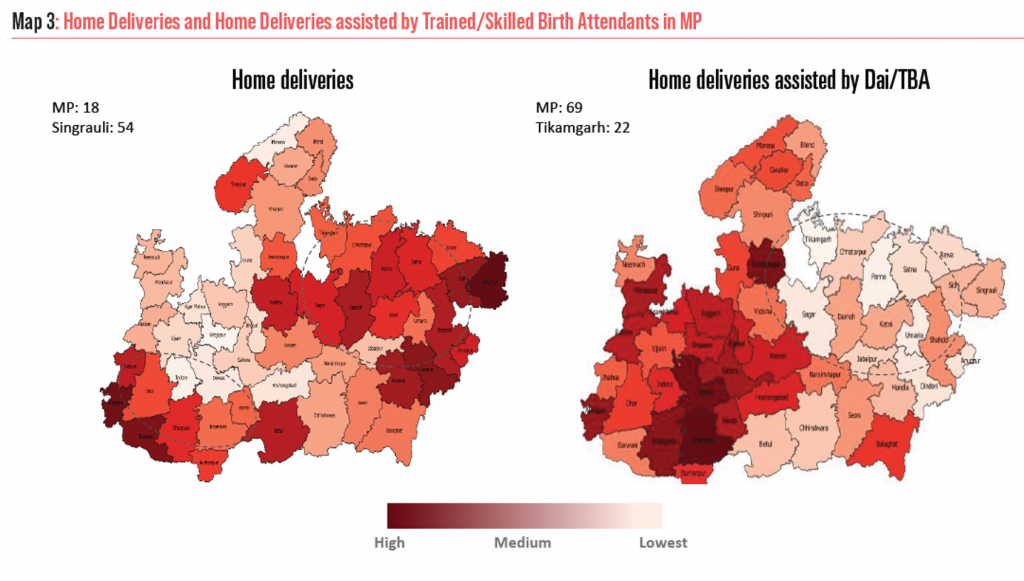
NFHS-4 district level analysis indicates that there are high proportions of home deliveries with low proportions attended by skilled birth attendants in NE MP (Map 3).
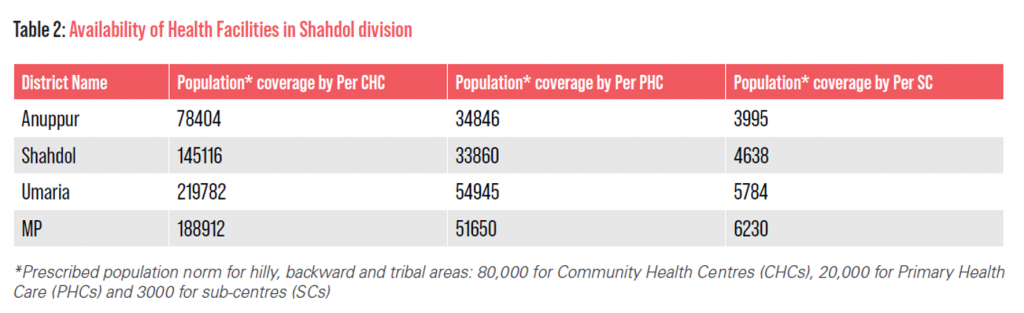
The availability of health facilities in Shahdol division is sub-optimal (Table 2). In most districts of the division, the population coverage of facilities is higher than the prescribed norms.
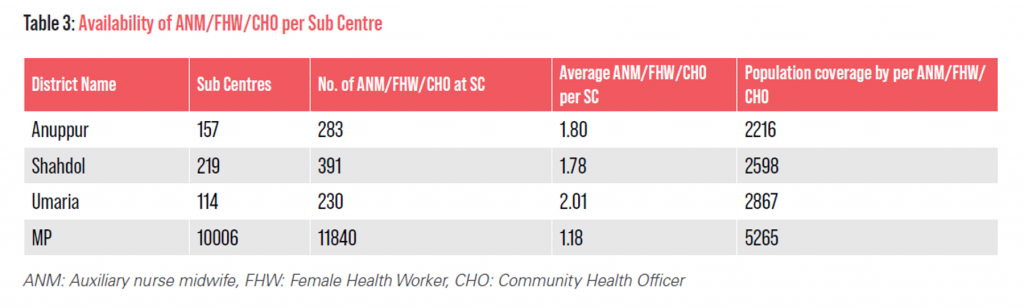
Even though the population covered by each ANM appears to be as per norm, she looks after twice the number of sub-centres than that prescribed in all three districts in Shahdol division (Table 3), suggesting a need to support travel or increase the numbers.
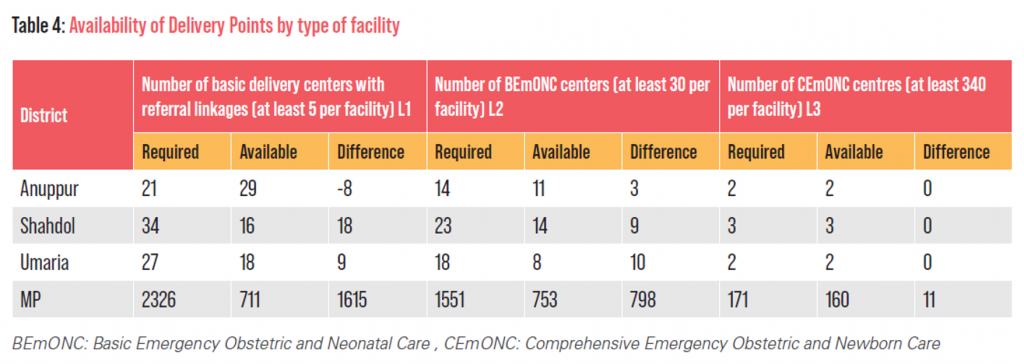
Similarly, the numbers of delivery centers, both for Basic Emergency Obstetric and Neonatal Care (BEmONC) centers and Comprehensive Emergency Obstetric and Newborn Care (CEmONC) centres in Shahdol and Sagar Division are inadequate (Table 4).
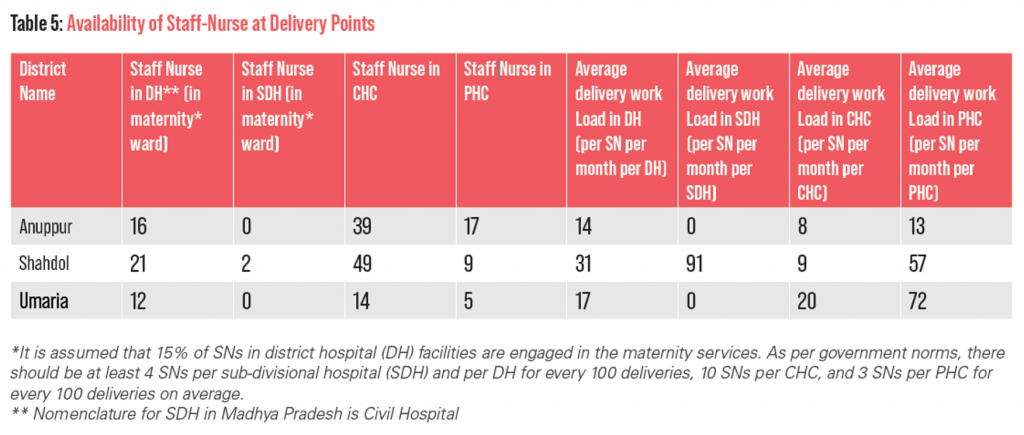
The availability of Staff-Nurses (SNs) at delivery points against the average delivery load is inadequate in two of the three districts (Table 5).
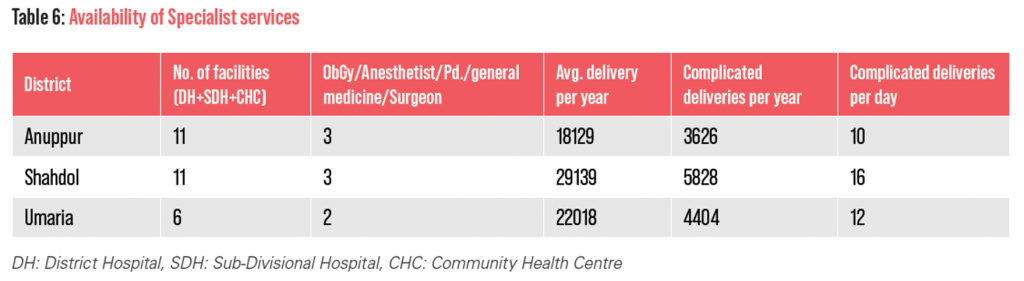
The availability of Specialists [Obstetrics and Gynaecology(OBG)/ Anaesthetist/Paediatrics/General Medicine/ Surgeon] in the districts of Shahdol and Sagar division are also inadequate (Table 6). A per government norms there should be at least one OBG and other specialists in every DH, SDH and CHC.
• The annual rate of reduction in MMR and NMR lags behind in MP, especially within NE divisions of MP
• The coverage of key community interventions (ANC and PNC services) can be enhanced by building upon platforms such as the VHND and improving human resource availability and competencies
• Improvements in the availability of health facilities and the numbers of human resources, especially specialists, need special focus in the tribal districts.
• Home delivery must be reduced and attended to by skilled birth attendants.
• A cohort analysis or serial cross-sectional surveys could help track behaviors among pregnant women and health care providers that would help understand changes in service utilization over time.
• The quality of care data is largely lacking in settings of institutional or home delivery. Availability of these data would further help to enhance our understanding.
• Certain analysis is based on NFHS-4 data and refers to a period 6-7 years ago. However, as the NFHS-5 is made available, a similar analysis would provide updated information on the current situation.
• Information on the availability and utilization of emergency medical transportation and the availability of private sector facilities for emergency obstetric and newborn care, under the PMJAY scheme was not included in the analyses.
Madhya Pradesh will need to accelerate the AARC in MMR to 6.8% to reach the SDG 2030 target of less than 70 Maternal Deaths per 100,000 live births, and an AARC in NMR to 8.6% to reach the SDG 2030 target of less than 12 Neonatal Deaths per 1000 live births. Focused interventions in the North-East parts of Madhya Pradesh, among tribal populations, especially within the Shahdol division could help to accelerate improvement in maternal and newborn health outcomes in this region and state-wide.
1World Health Organization: Reconciling maternal, newborn and child health with health system development. World Health Report ‘Make every mother and child count’ Geneva, Switzerland: WHO; 2005.
2Nair H, Panda R. Quality of maternal healthcare in India: Has the national rural health mission made a difference? J Glob Health. 2011;1:79–86.
3Shahdol Division: Anuppur, Shahdol, Umaria districts
4Sagar Division: Chhatarpur, Damoh, Panna, Sagar, Tikamgarh districts