Background
Sex work patterns have undergone a change owing to technology and social media1. Apart from the existing traditional street, brothel and home-based sites of solicitation, there are now new physical spaces such as Massage Parlours or Spas where solicitation takes place. Studies conducted in massage parlours in Asia and North America have indicated that masseurs and masseuses frequently engage in high risk behaviours including sex work which make them vulnerable to contracting HIV and other STI2,3,4. The evidences highlight that intervening at Spas and Massage Parlours are critical to enhancing coverage of HIV prevention, treatment and care services2,3,4. In India too, sex work dynamics have changed! Physical spaces such as Spas and Massage Parlours have emerged as new spaces for solicitation1. Hence, there is an urgent need to reach out to the FSWs and MSMs associated with the Spas and Massage Parlours for HIV related prevention, treatment and care services in India.
The Scenario in Delhi National Capital Territory
DSACS and DL TSU conducted rapid assessments to understand the HIV service needs of FSWs5 and MSMs6 involved in sex work through Spas and Massage Parlours in Delhi National Capital Territory (NCT). From the assessments, it was clear that the FSWs and MSMs who provide sex through Spas and Massage Parlours are at high risk of HIV and STI. This high-risk group, however is not covered by the traditional Targeted Intervention (TI) HIV prevention program. Therefore, designing HIV Interventions focusing on FSWs and MSMs involved in sex work through Spas and Massage Parlours would be essential to bridge the gap between this population and HIV services.
In response to the need to reach FSWs and MSMs working at the massage parlours with HIV prevention and care services, DSACS with the support of DL TSU, designed a bespoke strategy with the following objectives:
HIV Intervention in Spas and Massage Parlours
The HIV intervention was implemented to reach out to the FSWs and MSMs involved in sex work through Spas and Massage Parlours (SMPs). The beneficiaries of the intervention were – SMP Operators (SMPOs) and FSWs and MSMs associated with SMPs and involved in sex work in the premises.
| SMPOs: Individuals who are either managers or owners of SMPs; are directly involved in day-to-day operations and are in regular touch with FSWs and MSMs working in the SMPs. |
| FSWs and MSMs: In the context of the present implementation note, FSWs and MSMs who are involved in sex work through SMPs. |
| SMPO Counsellors: Individuals recruited to reach out to SMPOs and sensitize them on the TI Program. |
| KP Counsellors: Individuals responsible to provide counselling to the Key Population within the TI Program ambit. |
Geography
Five FSW TIs and one MSM TI are implementing the HIV prevention program covering following districts of Delhi NCT, where the concentration of SMPs where sex work is prevalent, is high – Central Delhi, East Delhi, North West Delhi, South Delhi, South East Delhi, and West Delhi.
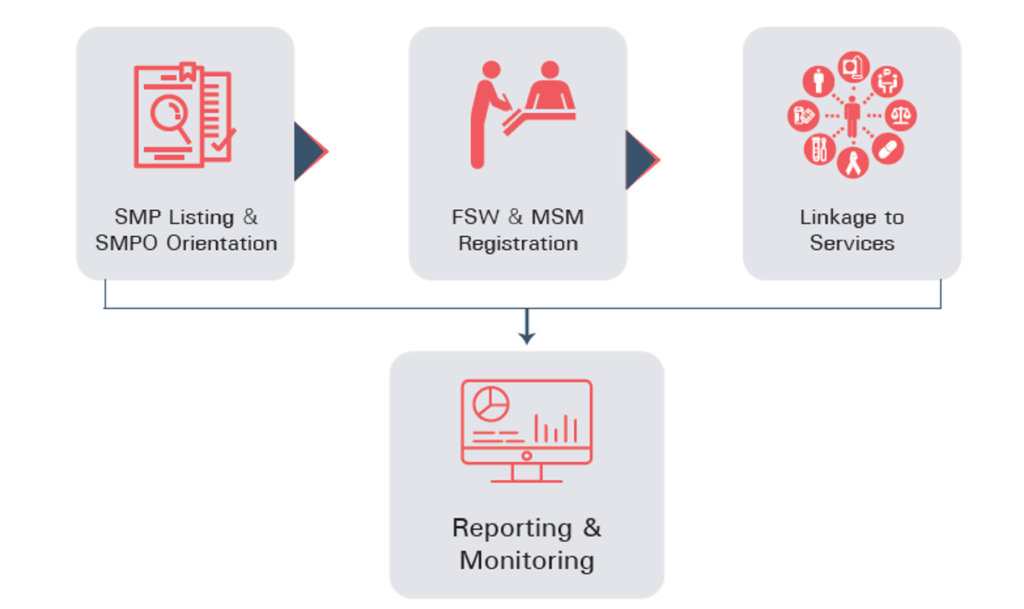
The following stages were adopted in the program (Figure 1). Monitoring and reporting was a crosscutting activity in all stages.
Results
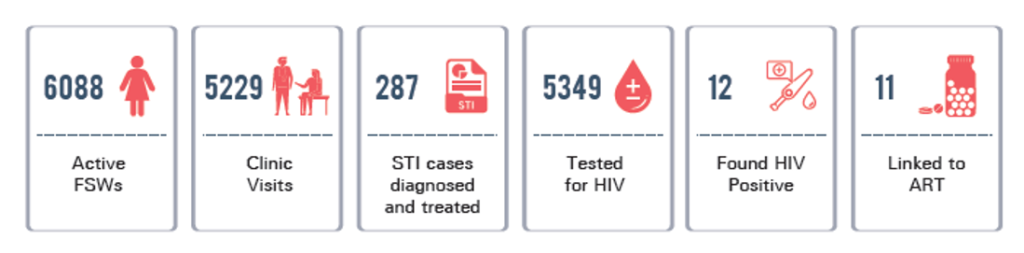
There were 6088 FSWs registered in TI. 5229 FSWs were provided clinical services; out of these, 287 FSWs reported STI symptoms and were subsequently treated. Out of the 088 FSWs, 5349 FSWs were screened for HIV; out of which, 12 FSWs were found HIV positive. Consequently, 11 FSWs were linked to ART (Figure 2).
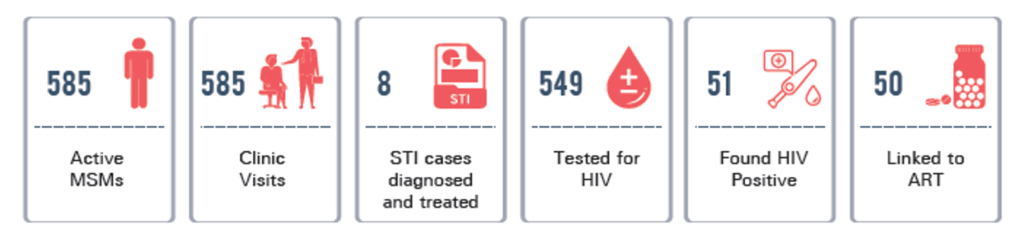
There were 585 MSMs registered in TI, 585 MSMs were provided clinical services; out of these, 8 MSMs reported STI symptoms and were subsequently treated. Out of the 585 MSMs, 549 MSMs were screened for HIV; out of which, 51 MSMs were found HIV positive. Consequently, 50 MSMs were linked to ART (Figure 3). The positivity in MSMs has been found to be higher as compared to that in the FSWs.
Learnings
Fostering a healthy relationship with the SMPOs consequently led to building trust and confidence of the FSWs and MSMs in the TI Program. The process of rapport building takes significant time and effort – maintaining confidentiality and sensitivity to the SMPOs was essential to establishing their willingness to collaborate towards playing a facilitative role in the HIV Intervention. Outreach activities when conducted with respect, empathy and a non-judgemental attitude, stimulate demand for services and the beneficiaries are more likely to seek services and benefit from the prevention, treatment and care interventions they need. Thus, deriving a meaningful participation from the SMPOs as well as FSWs and MSMs was the crux of bringing sustainability in the intervention.
There is an emergence of new SMPs across Delhi while some SMPs close temporarily or permanently or relocate. In order to deal with this highly dynamic nature of the sex work setting, adopting a snowballing approach to reach out to SMPs and FSWs & MSMs, ensures that the SMPOs are enrolled into the
HIV Education Program at the earliest and subsequently the FSWs and MSMs are reached out with the necessary services.
Apart from HIV/STI related needs, the FSWs and MSMs also shared about their over-all health, social and legal concerns – general health issues, social boycott, domestic violence, to name a few. This calls for a strategy that can cater to general health and social and legal protection needs of the FSWs and MSMs.
Challenges
Coverage and saturation of the FSW and MSM population under the HIV Intervention in SMPs is a challenge due to high mobility of the populations within and across SMPs in Delhi. Even after rigorous efforts and snowball approach, reaching out to every member of the population and linking them to the required services remains a challenge. The SMPOs are hesitant in facilitating the process of condom distribution among the FSWs
and MSMs associated with them. Two major reasons have been shared by the SMPOs: (i) Stocking condoms/contraceptives poses a legal threat as national laws prohibit sex work; these activities are prevalent in SMPs in a hidden manner. (ii) FSWs and MSMs are not allowed to carry condoms and if they intend to use them during sexual intercourse, they are expected to buy the same from the SMPOs; so, the SMPOs sell condoms to the population at a higher rate than the market and in turn earn a profit. This poses another risk for contracting HIV/STI as the FSWs and MSMs may not prefer to spend extra money on condoms and instead indulge in unprotected sexual intercourse. The duplication of SMPOs, FSWs and MSMs within TIs is identified and resolved through the lead tracker mentioned in the monitoring section. However, capturing duplication between the TIs has been a challenge.
Way forward
The HIV Intervention with the SMPs in Delhi has shown promising early results. The Intervention will further explore on building capacities of SMPOs to act as program intermediators in service delivery aspects like conducting HIV screening using CBS kits, educating the FSWs and MSMs on safer sexual practices and encouraging them to seek services like regular medical check-ups, HIV and syphilis testing and treatment for PLHA. The program also intends to train them in HIV awareness generation activities to be carried out with FSWs and MSMs associated with them, using digital and social media based applications. The program will explore the possibility to develop a centralized mechanism of service delivery and linkage, wherein, the FSWs and MSMs can register and opt for services at any given location irrespective of the TI they are registered with. This system will bridge the existing gap between FSWs & MSMs and the services. The FSWs and MSMs have experienced violence from clients as well as partners and hence they are in need of social and protection services. To address the need, collaborations have been planned with medical colleges, government departments and legal aid centres/ entities to ensure linkage of the population with these services. This will be instrumental in providing integrated, comprehensive, effective and affirming health-care services to the FSW and MSM population.
1Identifying changing trends In the sex work dynamics among Female Sex Workers (FSWs) in India
3Condom Use Among Men Who Have Sex With Men and Male-to-Female Transgenders in Jakarta, Indonesia
5Understanding the HIV service needs of FSWs working in the Massage Parlors/Spa in Delhi: A Rapid Assessment, DSACS & DL TSU, 2018-2019
6Understanding the HIV service needs of MSMs working in the Massage Parlors/Spa in Delhi: A Rapid Assessment, DSACS & DL TSU, 2018-2019